From refugee camps in Kenya or Jordan to countries in conflict such as Yemen or Syria, the expertise of humanitarian actors is key to limiting the spread of the pandemic in countries where health systems are fragile. In order to better define the stakes and the different tools that can be mobilised, the new Covid-19 Humanitarian platform allows the systematic production of orientation documents and the sharing of lessons learned for a better impact of humanitarian programmes.
While the intensity and celerity of the coronavirus transmission were no surprise for public health experts, health systems were not ready for it. Increased international mobility has transformed the outbreak into a pandemic, which has touched rich and poor countries with the same intensity. While the United States and the United Kingdom are still struggling to contain the virus transmission, Brazil and Russia are emerging as new epicentres of the pandemic alongside other emerging hotspots in Africa. In June 2020, while the virus was making its way to South America, new cases were discovered in Yemen and Cox’s Bazar refugee camp, Bangladesh.
According to the United Nations High Commissioner for Refugees (UNHCR), amongst the 100 countries affected by the virus as of March 10th, 30 of them had a refugee population exceeding 20,000[1]UNHCR, “UN Refugee Agency steps up COVID-19 preparedness, prevention and response measures”, 10 March 2020, … Continue reading. The recent information received from two refugee camps, one in Kenya and another in Jordan, reports that the camps are closed and any movement in or out is restricted. Access to safe drinking water has been reduced due to the decrease of water tanks entering the camp. It took some time before refugee populations received clear information from authorities on the measures to be implemented to reduce transmission – a delay that has contributed to the spread of rumours and misinformation, generating fear amongst the population. This situation truly demonstrates the low level of preparedness currently in place in potentially high-risk places, where populations are overcrowded, hygiene and living conditions are challenging and where access to water and soap has become difficult.
In a way, many countries in “the third wave” such as those on the African continent have had time to put in place the right measures to prevent transmission, detect cases and manage confirmed cases. Following the pandemic’s progress from China to Europe, many African countries successfully established policies even before the first case was detected. Worldwide, a total of 215 countries and territories have reported Covid-19 cases. In June 2020, one country, Rwanda reported deaths for the first time. At 2 June 2020, a total of 152,442 Covid-19 cases and 4,334 deaths (case fatality rate of 3%) were reported in 54 African countries[2]African Union, “Outbreak Brief #20: Coronavirus Disease 2019 (COVID-19) Pandemic”, 2 June 2020, … Continue reading, representing about 2.5% of all cases reported globally.
While the pandemic progresses around the world, we are concerned that countries with weaker health systems may find it difficult to implement appropriate procedures and services. The situation in war-torn Yemen, where the first case of Covid-19 was confirmed on 15 May, is very worrying with the death toll attributed to Covid-19 increasing daily. In Bangladesh, the total bed capacity provided by humanitarian actors will reach 1,100 by mid-June, contributing to the aim of at least 1,900 beds in the Cox’s Bazar District. However, modelling projections for Cox’s Bazar indicate that as many as 10,000 hospital beds may be needed at the peak[3]Shaun A. Truelove et al., “The Potential Impact of Covid-19 in Refugee Camps in Bangladesh and Beyond: a modeling study”, medRxiv, https://doi.org/10.1101/2020.03.27.20045500.
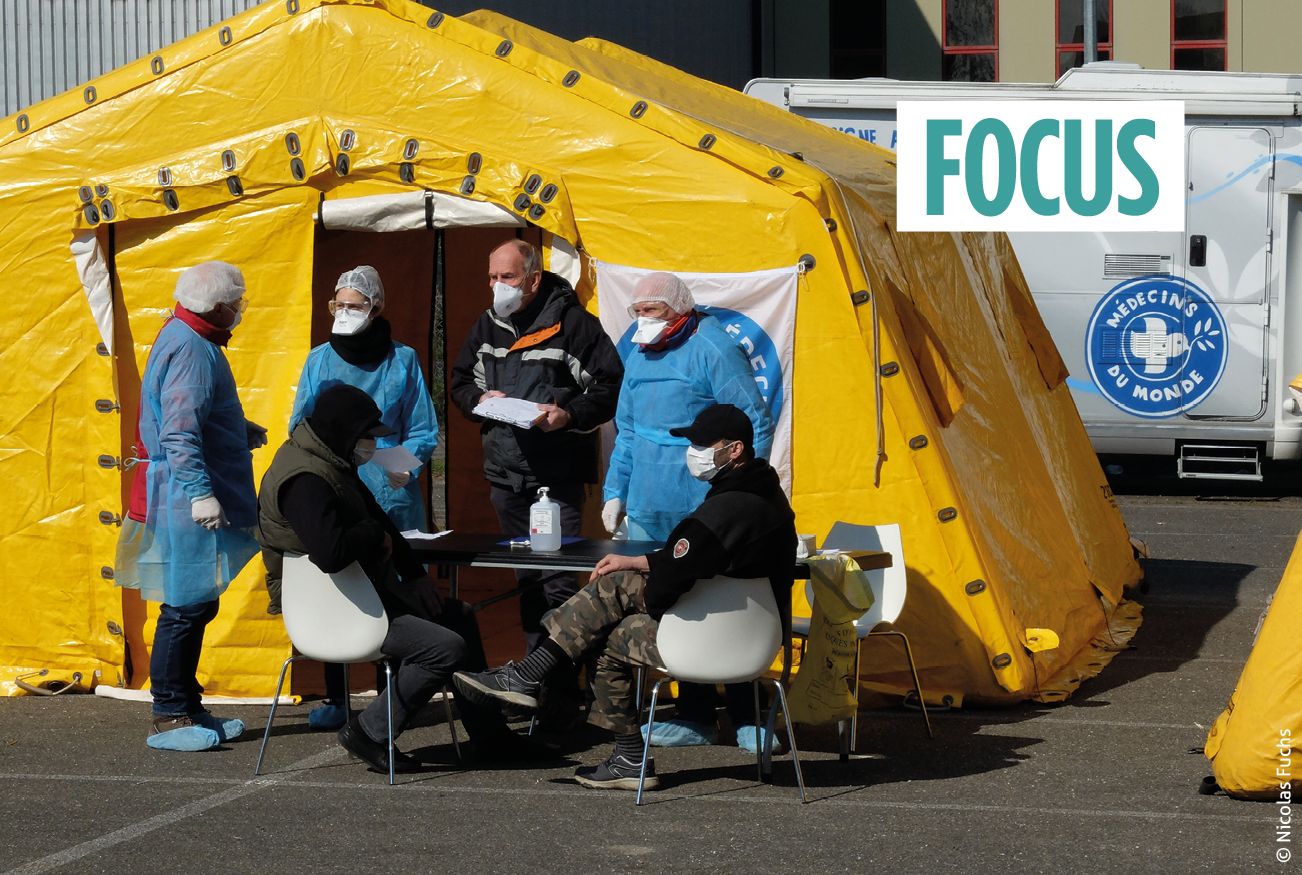
Humanitarian organisations can play a key role in supporting national authorities. As with every pandemic, time is of the essence, and in such cases, the humanitarian response has the added value of being able to deploy the right resources and the right expertise to the right places. One of the key strategies used to good effect in China and European countries has been the creation of field hospitals for triage cases or the use of community health workers for contact tracing. Humanitarian organisations are very experienced in this field and were able to construct these in vulnerable countries to get ahead of the curve.
| Preparing, responding and adapting existing programmes to Covid-19 in humanitarian settings: the Covid-19 Humanitarian platform
Alex Odlum – Research Coordinator, Geneva Centre for Education and Research in Humanitarian Action Humanitarian actors are innovating and adapting their programmes in order to address the specific impacts of Covid-19 and maintain safe and effective humanitarian services in rapidly changing contexts. The Covid-19 Humanitarian platform seeks to establish guidance for humanitarian actors making these adaptations and share and learn from their experiences in the field. Since March 2020, three universities – The Johns Hopkins Center for Humanitarian Health, the Health in Humanitarian Crises Centre at the London School of Hygiene and Tropical Medicine and the Geneva Centre for Education and Research in Humanitarian Action – have been conducting research to investigate how humanitarian programmes are changing in light of Covid-19. Adaptations and innovations have been categorised under the following three domains: preparing for and responding to Covid-19, adapting existing interventions and cross-cutting issues. |
We are concerned that countries with weaker health systems may find it difficult to implement appropriate procedures and services.
Preparing for and responding to COVID-19
The first domain includes specific interventions to prepare for Covid-19 in a humanitarian crisis context, or to respond to Covid-19[4]Ibid. where cases are already confirmed. For example, to assess the risks of Covid-19 and the needs of refugees and migrants on the move, the Mixed Migration Centre’s “Mixed Migration Monitoring Mechanism Initiative” (4Mi) specifically designed and deployed a new phone-based survey to provide crucial information for humanitarian response without having enumerators physically collecting data on the ground. Another specific intervention has been to set up a comprehensive investigation and surveillance system across Afghanistan, with 34,000 local volunteers re-assigned to notify 34 Rapid Response Teams of suspected Covid-19 cases in their area. Additional testing, border screening, training and risk communication complement this intervention.
A wide range of interventions have been implemented to raise public awareness in communities, communicate risk and silence rumours, using a range of both traditional and technology-based strategies, from megaphones and radio to WhatsApp and Facebook broadcasts. In Pakistan, for example, the International Rescue Committee (IRC) has set up remote risk communication and community engagement procedures. In health facilities, interventions have bolstered infection prevention and control, made space for suspected cases to be isolated, or established triage and prioritisation mechanisms to manage caseloads effectively. MSF have restructured their services in overcrowded refugee and migrant camps on Lesbos island in Greece to prepare for potential Covid-19 cases. The American Refugee Committee in Somalia set up triage mechanisms and hospital referral services across 15 primary health clinics which they operate in partnership with the Ministry of Health.
Adapting existing interventions to Covid-19
The Covid-19 pandemic is defining a new normal, which requires existing humanitarian interventions to be adapted or redesigned to prevent and reduce transmission of the virus. In many humanitarian contexts, a difficult trade-off is presented between maintaining essential services and limiting contact between individuals (among both community members and staff). Solutions include prioritising critical services by ensuring access for population groups in most urgent need, while limiting access for others and finding innovative ways to serve them. In the Bekaa Valley in Lebanon, MSF was able to adapt its non-communicable disease services for Syrian refugees by setting up remote consultations on the phone, remote medicine collection points in strategic locations and a referral system to ensure access to care for the most severe cases when needed.
Retraining staff and repurposing facilities have also helped to meet additional Covid-19 needs, while continuing essential services in terms of health, food security, water, sanitation and hygiene (WASH), nutrition, education and other humanitarian services. In Pakistan, for example, the IRC has emphasised capacity building and staff safety while working to maintain critical reproductive health services.
Cross-cutting issues
Covid-19’s far-reaching impact has also affected many cross-cutting areas of humanitarian operations, including coordination, ethics, protection, gender, logistics, monitoring and evaluation and attacks on healthcare. Coordination mechanisms have had to adjust to new constraints, actors, and funding priorities. Logistics and supply chains have been ruptured by transport restrictions and stock shortages, requiring innovative solutions. For example, in Myanmar, the IRC adapted to supply constraints by employing women’s groups to produce cloth masks and face shields for community members and medical teams. Gender and protection mainstreaming remain as important as ever, but are having to navigate shifting circumstances; for example, the protection needs of the elderly and people at risk of sexual and gender-based violence have escalated due to Covid-19. In addition, the changing nature of risks and vulnerabilities gives rise to new ethical concerns, such as the duty of care to staff exposed to the virus.
Across all three domains, Covid-19 is changing the nature of humanitarian action. Many actors have been quick to compile useful resources to guide specific audiences through the crisis. While the global consolidation of knowledge resources offers an invaluable tool for humanitarian responders, lessons from the field – including when and why to depart from the guidance, be pragmatic, innovative and reactive – also need to be captured in real time and fed back into the global information cycle so as to inform current and future humanitarian responses. By providing context-specific field experiences alongside global guidance selected by public health experts, the Covid-19 Humanitarian platform aims to bring both global and local perspectives together towards our common goal.
The website of the Covid-19 Humanitarian Platform: www.covid19humanitarian.com
If you are a humanitarian actor and you wish to share your experiences you can contact the platform via its website or using the following e-mail address: covid19humanitarian@gmail.com
This note was written with the support of Orit Abrahim, Chiara Altare, Karl Blanchet, Caroline Favas, Neha Singh and Paul Spiegel.
Prioritise essential interventions
There are many questions related to current humanitarian activities about which interventions should be prioritised. There is no doubt that it cannot be business as usual. Humanitarian organisations and governments need to redistribute their health staff to be able to respond to the pandemic and postpone some non-essential health interventions. However, many essential and routine operations need to be protected and continued. In a recent study with an expert panel, we at the Geneva Centre of Humanitarian Studies identified a set of 93 interventions that must continue and are considered urgent for patients. These include interventions related to mother and child health and nutrition, along with services for chronic care patients (HIV, hypertension and diabetes) to name just a few. Governments and humanitarian organisations need to conduct a rapid priority exercise to postpone some activities so that staff can be reassigned to case detection and management while ensuring that essential health services are delivered.
Humanitarian organisations and governments need to redistribute their health staff.
Protect healthcare staff
It is a priority for government and humanitarian organisations to protect healthcare staff by providing them with Personal Protective Equipment (PPE) when caring for patients with a confirmed or possible Covid-19 infection. This requires mass orders for the right equipment. The World Health Organization (WHO) and a few relief agencies have prepositioned PPE kits in order to support the case management of the first 200 cases in priority countries. Accessing a large amount of PPE has become very challenging. It is important to be very transparent with health care workers about the potential risks they face if there is a shortage of PPE as the Ebola outbreak in West Africa has shown[5]Eduardo A. Undurraga et al., “Potential for broad-scale transmission of Ebola virus disease during the West Africa crisis: Lessons for the Global Health security agenda”, Infectious Diseases … Continue reading.
Prevent
Prevent, detect and manage are the three pillars of the public health strategy to tackle the pandemic. We know that social distancing is very effective at avoiding the spread of the virus. This requires avoiding any mass gatherings and respecting a two-metre distance between individuals. While all refugee camps have been closed to prevent external visitors from introducing the virus, the situation in Cox’s Bazar or in hotspots in Greece is very worrying in an environment where physical distancing within and between families remains very difficult. As we now know, hand washing is very effective in controlling the transmission of the virus, but in many refugee camps, slums and remote villages, running water and soap are not available. It is therefore urgent to install water stations with soap in all overcrowded places. The level of knowledge of local populations about preventive measures is very high in most places thanks to local media, local NGOs and community health workers but the implementation of these measures remains very difficult in many humanitarian situations.
Detect and manage cases
A key priority for managing cases is testing. However, this requires access to tests, which are currently allocated on a priority basis to the most affected countries. Setting up a testing campaign requires clear protocols, laboratory capacity and triage on site. Many countries such as China, France and Switzerland have created triage field hospitals outside the main hospitals to separate confirmed cases from suspected cases. Large humanitarian organisations have stocks of field hospitals that can be rapidly deployed to sites. The management of severe cases in intensive care units (ICUs) requires, in particular, the use of ventilators, of which there is currently a chronic shortage and a high level of medical expertise. 50% of the African ICU capacity is in South Africa, illustrating a lack of capacity in the continent’s different countries.
Global governance will need to negotiate the antagonisms between the private sector and the notion of public good.
Time for international collaboration, not selfish nationalism
Travel bans and border closures are a concern for the continuation of humanitarian operations in the most acute crises such as Yemen and Syria. Around us we are witnessing an increased solidarity between neighbours and citizens, with widespread recognition of the importance of healthcare workers in our society. However, the rise of nationalism and protectionism is a concern at a time when we need international cooperation to make sure everyone can cope. We are eagerly awaiting a new vaccine, but availability and distribution must be guided by clear and transparent principles far from the simple “the richer you are, the earlier you have access to the vaccine”. These principles need to be fair and take into account the burden of disease on the most disadvantaged populations[6]Nuffield Council on Bioethics, “Fair and equitable access to Covid-19 treatments and vaccines. Rapid policy briefing”, May 2020, London.. Global governance will need to negotiate the antagonisms between the private sector and the notion of public good, which will certainly lead to a power struggle between different governments and between governments and the WHO. There is no doubt that humanitarian organisations will play a key role in ensuring fairness regarding the distribution of vaccines to the most disadvantaged populations
Post-Covid-19
There is no doubt that the field of public health has been under great strain during the pandemic. It has shown signs of weakness, unpreparedness and a global governance led by the WHO which has been shaken by the departure of the USA. We will need to rethink and redefine the notion of public good in times of pandemics and expound a set of principles promoting equity and fairness to protect the most vulnerable populations, especially those living in conflict-affected countries.
ISBN of the article (HTML) : 978-2-37704-694-2 |